Cervical Cancer
Cervical Cancer Screening
What is Cervical Cancer?
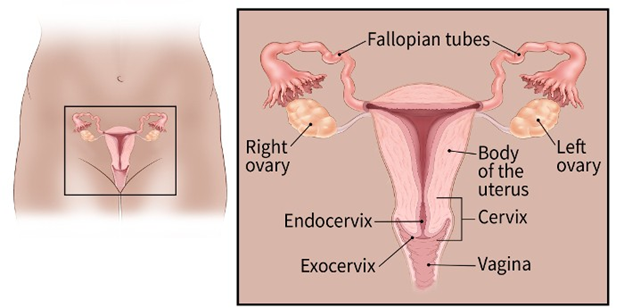
Cervical cancer is a disease in which malignant cells form in the tissue of the cervix. The cervix connects the vagina (birth canal) to the uterus (or womb). There are two parts of the cervix, and they contain different types of cells. The endocervix is the opening that leads into the uterus, which is made up of glandular cells. The exocervix is the outer part of the cervix, and consists of squamous cells. This is the part of the cervix that is observed when a doctor uses a speculum during a wellness exam. Cervical cancer occurs when the cells that line the cervix start to grow out of control. Most cervical cancers begin in what is called the transformation zone. This is the part of the cervix where these two cell types meet.
From: What Is Cervical Cancer? | American Cancer Society
Facts about Cervical Cancer
Over the past 40 years, incidence and mortality have decreased significantly, thanks to early detection and regular screening.
What are the Types of Cervical Cancer?
For some individuals, pre-cancerous cells continue to mutate into an invasive, true cancer.
- Squamous cell carcinomas are the most common type (up to 90% of all cervical cancers), which often develop in that transformation zone. (Squamous cells are thin, flat cells that look like fish scales, and are found in the tissue that forms the surface of the skin, the lining of the hollow organs of the body, and the lining of the respiratory and digestive tracts.)
- The second most common are adenocarcinomas, which develop from the glandular cells in the endocervix. (Glandular cells are involved in the menstrual cycle and in the production of cervical mucus.)
- The least common type are adenosquamous (“mixed”) carcinomas, which have features of both types of cells.
How Does Cervical Cancer Develop?
Cervical cancer develops when normal cells begin to develop mutations. During this process, the cells may begin to develop abnormalities as they transform into cancer cells. A term used to describe the presence of abnormal cells within a tissue or organ is “dysplasia”. Dysplasia is not cancer, but it may sometimes become cancer. There are several terms that describe this pre-cancerous transformation.
Cervical intraepithelial neoplasia (CIN) is graded on a scale of 1-3, based on how abnormal the tissue appears.
- CIN1 is sometimes called mild dysplasia, or low-grade squamous intraepithelial lesion. That means the tissue looks mildly abnormal, but is classified as pre-cancerous because it is the least severe in terms of changes in the tissue.
- CIN2 is a moderate dysplasia, so the tissue has become more abnormal in its structure.
- CIN3 is a severe dysplasia, or a high-grade squamous intraepithelial cell lesion. In CIN3, the tissue is extremely suspicious in appearance, so this is considered to be a serious pre-cancer.
What are the Symptoms of Cervical Cancer?
Many individuals with early stages of cervical cancer or pre-cancers have no symptoms. Symptoms are more common when the cancer is later stage, and therefore larger and more advanced. These symptoms may include:
- Abnormal vaginal bleeding or spotting
- Unusual vaginal discharge
- Pain during intercourse
- Pelvic pain
- Swelling of the legs
- Problems urinating or having a bowel movement
- Blood in the urine
Since symptoms usually aren’t evident until later, less treatable stages, this is why regular screening is so important!
How Can I Detect Cervical Cancer Early?
Not all individuals with pre-cancers will develop cervical cancer. That’s the good news. These pre-cancer lesions are very treatable if caught in an early stage. The best way to detect these treatable pre-cancers is to be screened regularly.
- Pap test – The Pap test, or Papanicolaou smear, is a procedure that collects cells from the cervix and looks at them under a microscope. This test is sometimes called “cytology.” The doctor will place a metal or plastic instrument called a speculum inside of the vagina. This keeps the vagina open so the cervix is easy to see. The health care professional will use a small brush to collect or scrape cells from the exocervix, which can be looked at under a microscope.
- HPV test – Because most cervical cancers are caused by specific types of HPV, testing for infection with these types of HPV is now the preferred test for cervical cancer screening.
- Primary HPV testing: Individuals who are 25-65 years of age can undergo primary HPV testing every 5 years. If the HPV test is negative, current recommendations state that the cytology (Pap test) is not necessary.
- Secondary HPV testing: If primary HPV testing is not available, HPV testing combined with cytology once every 3 years is recommended.
Cervical Cancer Screening Resources
Women who are concerned about the cost of receiving a screening mammogram or Pap test from their health care provider may have resources available to them to assist with covering this expense: Medicare Part B and Missouri’s Show Me Healthy Women program offer free breast and cervical cancer screenings for women who qualify.
Medicare Part B
Medicare is the federal health insurance program for people who are 65 or older; for certain younger people with disabilities; and for people with End-Stage Renal Disease, which is permanent kidney failure requiring dialysis or transplant.
Medicare Part B will cover 100% of the cost of a Pap test, a pelvic exam, and a breast exam for eligible participants once every 24 months.
Participants may be eligible for these screenings every 12 months if found to be at high risk for cervical cancer or are of childbearing age and have had an abnormal Pap test in the past 36 months.
Show Me Healthy Women
The Show Me Healthy Women program offers free breast and cervical cancer screenings for Missouri women who meet certain eligibility requirements. Women who have an income at or below 200 percent of the federal poverty level for household income; are aged 35 to 64 or older; do not receive Medicare Part B; and do not have insurance to cover program services qualify for Show Me Healthy Women program benefits.
To locate a participating health care provider, visit Show Me Healthy Women or call 866-726-9926.
Cervical Cancer Prevention
What are the Risk Factors for Cervical Cancer?
Nearly all cervical cancers are caused by HPV, but not all individuals who have HPV will develop cancer. This is where HPV screening can help you understand your risk. Some types of HPV are more likely to cause cervical cancer, so testing to see if you have one of these high-risk types of HPV will help you understand your risk of developing cervical cancer.
While HPV is the main risk factor, other risks include:
- HIV - Being HIV positive can increase your risk of cancer because your immune system issuppressed and it is more difficult for your body to fight off infections and cancer cells.
- Chlamydia infection – Chlamydia is a sexually transmitted infection. Some research suggests that Chlamydia bacteria helps HPV grow on the cervix, which increases cancer risk.
- Smoking – Tobacco use increases the risk of cervical cancer, as well as many other types of cancer.
- Birth control pills – Use of birth control pills for five or more years may increase your risk, but that risk decreases when oral contraception use stops.
- Multiple children – Women with three or more biological children are at increased risk, possibly because of hormonal changes during pregnancy or the fact that pregnancy affects the immune system and may allow the HPV infection to stick around longer.
- Having multiple sexual partners – Sexual activity increases risk of cervical cancer because it increases the chances of becoming infected with multiple types of HPV.
- Diethylstilbestrol (DES) – This drug was prescribed to some pregnant women from 1938 to 1971 to prevent miscarriage. Women whose mothers took DES while pregnant have an increased risk of clear-cell adenocarcinoma. About one in every 1000 women whose mothers took DES will develop cervical cancer (0.1%)
- Family history – If you have a sister or mother who had cervical cancer, your chances may be increased.
What Can I Do to Prevent Cervical Cancer?
- For maximum protection against HPV, vaccinate girls and boys between ages 9 to 12 with 2 doses of the vaccine, also known as Gardasil®9.
- If you are 26 years or younger consult your dentist or doctor about the vaccines for HPV. People ages 27 to 45 may also receive the HPV vaccines if considered to be at high risk for HPV infections.
- Regularly see the doctor for checkups that include cervical cancer and HPV screening. Early detection means better treatment outcomes if cancer is found.
- Be aware of your risk factors. Women are more likely to get cervical cancer as they get older.
- If you have a poor diet, eating more fruit and vegetables may decrease chances of developing many types of cancer, including cervical cancer.
- Stop using tobacco products and reduce or eliminate alcohol consumption to reduce the risk of cancer.
- Condoms used correctly and a new one used every time during sex can provide some protection. Condoms do not cover every possible HPV-infected area of the body. Condoms should be put on before any contact and kept on until sex is finished.
- Limit the number of sex partners and avoid sex with people who have had may other partners.
Cervical Cancer Treatment
What Happens if My Doctor Finds Something Suspicious?
Do not panic! The doctor may not be able to tell if what he or she is seeing is cancer or not. The doctor may refer you for testing the day of your checkup or after the second checkup.
Questions to Ask a Doctor Regarding Cancer
- What is my main problem?
- Why do you think what I have is cancer?
- Is there a chance I don’t have cancer?
- Would you please write down the kind of cancer you think I might have?
- What do I need to do?
- What will happen next?
- What tests will I need to have?
- Where will the test be done?
- Who can explain the tests to me?
- How and when will I get the results?
- Who will explain the results to me?
- What do I need to do next?
- Why is it important for me to do this?
For more questions go to American Cancer Society
Cervical Cancer Treatment
- Surgery - Most patients with cervical cancer will have surgery. This could include cryosurgery (freezing), laser surgery (burning), conization (cone biopsy) to remove a sample of the abnormal tissue in the cervix, or a hysterectomy to remove the uterus and cervix.
- Radiation therapy – Radiation uses high-energy rays to kill cancer cells. This could use an external beam aimed at the cervix or a radioactive source that can be implanted in the vagina, near the cervix (brachytherapy).
- Chemotherapy – Chemotherapy involves the use of drugs to kill the cancer cell. Chemotherapy is given in multiple rounds, and treatment often lasts for several months.
- Immunotherapy – Immunotherapy is a treatment to boost the immune system to help your body attack the cervical cancer cells.
Educational Tools & Resources
Resources to Support Cervical Cancer Survivors
Survivorship care plans help cancer patients that have completed treatment understand how to manage problems that can happen after treatment. Guidelines provide help on how to talk to dentists, doctors and other healthcare providers about follow-up care. Guidelines also have information on how to manage treatment effects.
- American Cancer Society’s Living as a Cervical Cancer Survivor
- Cancer.Net
- OncoLink
- Cancer Survivors
- Missouri Comprehensive Cancer Control Program’s Tips for Healthy Survivorship
What Happens After Treatment?
You will see your cancer doctor for years after your treatment ends. It is important that you go to all of the appointments. The exams and test can help find new cancer or returning cancer sooner, helping you get treatments sooner to stop the cancer.
Find a Provider
- Ask your dentist or doctor about the vaccine for HPV.
- Children who are eligible can receive free vaccines before their 19th birthday through the Vaccines for Children program
