Hepatitis C
Updates
- Provider Letter - Perinatally Exposed Infants Testing New
- Letter to Providers – Hepatitis C Recommendations
The Viral Hepatitis and Fatty Liver ECHO empowers and supports primary care providers to effectively and confidently treat patients suffering from liver diseases.
Overview
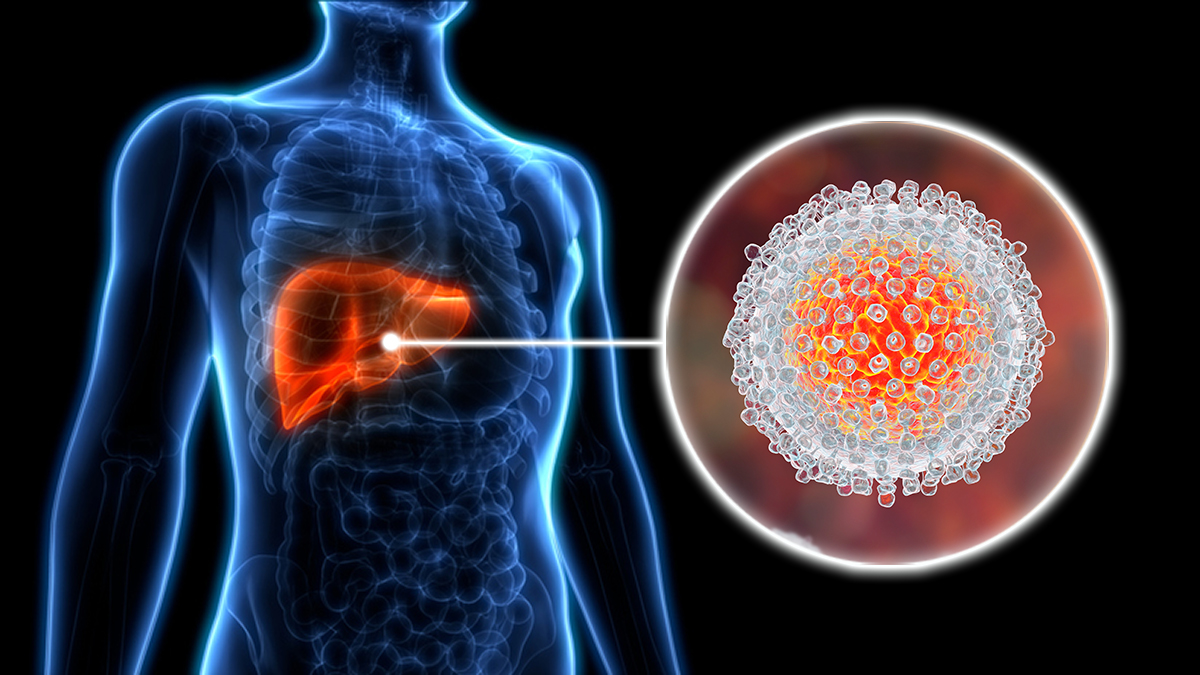
Hepatitis C attacks the liver but can remain without symptoms for decades. HCV is not vaccine preventable and is the most common blood borne infection in the United States (U.S.). According to the Centers for Disease Control and Prevention (CDC) an estimated 3-4 million persons in the U.S. have chronic Hepatitis C virus infection. Most people do not know they are infected because they don’t look or feel sick. Of those, it is estimated that 2.7 million are currently living with chronic HCV infection. HCV related Chronic Liver Disease (CLD) is the leading indication for liver transplant among adults in the United States.
HCV is most often spread by direct blood-to blood contact. HCV is usually spread when blood from a person infected with the Hepatitis C virus enters the body of someone who is not infected. The HCV can live in dried blood and on environmental surfaces for days. The virus can be spread easily to others through blood, even in amounts too small to see.
Symptoms

Approximately 70%-80% of people with acute Hepatitis C do not have any symptoms. Some people, however, can have mild to severe symptoms that occur from two weeks to six months after being infected, including:
- Jaundice (yellowing of the skin and/or eyes)
- Abdominal pain
- Fatigue
- Loss of appetite
- Unexplained weight loss
- Nausea and vomiting
- Low-grade fever
- Pale or clay colored stools
- Dark urine
- Skin rash
Risk Factors
- Baby Boomer - Born 1945-1965
- Injection Drug Use (IDU)
- Health-Care Setting
- Perinatal Transmission
- Tattooing and Piercings
- Sexual Contact
- Other Risks
Baby Boomer - Born 1945-1965
- People born from 1945-1965 are 5x more likely to have Hepatitis C. While anyone can get Hepatitis C, people born during these years are five times more likely to have Hepatitis C than other adults. That’s why CDC recommends everyone born from 1945-1965 get tested for Hepatitis C.
- The reason that baby boomers have high rates of Hepatitis C is not completely understood. Most boomers are believed to have become infected in the 1970s and 1980s when rates of Hepatitis C were the highest. Some ways baby boomers could have been infected from medical equipment or procedures before universal precautions and infection control procedures were adopted. Others could have gotten infected from contaminated blood and blood products before widespread screening virtually eliminated the virus from the blood supply by 1992. Sharing needles or equipment used to prepare or inject drugs, even if only once in the past, could spread hepatitis C. Still, many people do not know how or when they were infected.
- More information is available at Know More Hepatitis
Injection Drug Use (IDU)
The sharing of needles, syringes and other IDU equipment is the most common mode of HCV transmission in the US. It can also be spread by other drug use equipment (i.e, items used for snorting/straws, cottons, cookers, etc).
Past injection drug use is also a risk, including those who injected only one time or many years ago.
- For more information: HEPATITIS C & INJECTION DRUG USE
Health-Care Setting
HCV was commonly spread through blood transfusions and organ transplants before 1992 when widespread screening of the blood supply began. HCV was also spread through blood products (for clotting problems) made before 1987. HCV can be transmitted through needlestick injuries as well.
Perinatal Transmission
Transmission of HCV from infected mothers to infants occurs about 6% of the time. The CDC states that transmission risk is not related to the following:
- Delivery method, unless there is prolonged exposure to ruptured membranes and blood
- Breast feeding, unless nipples are cracked and bleeding
Tattooing and Piercings
Transmission of HCV is possible when poor infection-control practices are used during tattooing or piercing, or if the tattoo or piercing instruments are not sterilized correctly. HCV can also live in tattoo inks so they should never be re-used. Body art is becoming increasingly popular in the United States, and unregulated tattooing and piercing are known to occur in prisons and other informal or unregulated settings.
Sexual Contact
The CDC states that sexual contact is an “inefficient means” of HCV transmission, however sexual transmission is possible and the numbers of HCV infections traced to sexual transmission is growing. The likelihood of HCV transmission through sexual contact is related to the following:
- The number of lifetime sex partners
- A history of sexually transmitted diseases (STDs), especially the presence of an STD at the time of exposure to HCV
- Sex involving tissue trauma leading to exposure to blood
Other Risks can include:
- Sharing personal care items that may have come in contact with another person’s blood, such as razors, toothbrushes or nail clippers
- Inoculation practices involving multiple use needles or immunization air guns
- Exposure of broken skin to HCV infected blood
- HIV infected persons
People with current or past risk behaviors should consider HCV testing and consult with a physician. HCV testing is currently not available at most public health clinics in Missouri. For information about HCV testing that is available, call the HCV Program Coordinator at 573-751-6439.
Testing
Doctors use a blood test, called a Hepatitis C Antibody Test, to find out if a person has ever been infected with Hepatitis C. The Hepatitis C Antibody Test, sometimes called the Anti-HCV Test, looks for antibodies to the Hepatitis C virus. Antibodies are chemicals released into the bloodstream when someone gets infected.
Non-Reactive or Negative Hepatitis C Antibody Test
A non-reactive or negative antibody test means that a person does not have Hepatitis C.
- However, if a person has been exposed to the Hepatitis C virus in the last 6 months, he or she will need to be tested again.
Reactive or Positive Hepatitis C Antibody Test
- A reactive or positive antibody test means that Hepatitis C antibodies were found in the blood and a person has been infected with the Hepatitis C virus at some point in time.
- Once people have been infected, they will always have antibodies in their blood. This is true even if they have cleared the Hepatitis C virus.
- A reactive antibody test does not necessarily mean that you have Hepatitis C. A person will need an additional, follow-up test.
Persons for Whom HCV Testing Is Recommended
- Adults born from 1945 through 1965 should be tested once (without prior ascertainment of HCV risk factors)
- Those who:
- Currently inject drugs
- Ever injected drugs, including those who injected once or a few times many years ago
- Have certain medical conditions, including persons:
- who received clotting factor concentrates produced before 1987
- who were ever on long-term hemodialysis
- with persistently abnormal alanine aminotransferase levels (ALT)
- who have HIV infection
- who received clotting factor concentrates produced before 1987
- Were prior recipients of transfusions or organ transplants, including persons who:
- were notified that they received blood from a donor who later tested positive for HCV infection
- received a transfusion of blood, blood components, or an organ transplant before July 1992
- Currently inject drugs
- HCV- testing based on a recognized exposure is recommended for:
- Healthcare, emergency medical, and public safety workers after needle sticks, sharps, or mucosal exposures to HCV-positive blood
- Children born to HCV-positive women
Note: For persons who might have been exposed to HCV within the past 6 months, testing for HCV RNA or follow-up testing for HCV antibody is recommended.
Treatment
For the latest treatment guidelines, see CDC’s website at: Hepatitis C | CDC.
Persons who receive and early diagnosis of HCV infection and receive care are more likely to have a sustained virological response (SVR - meaning that the virus is not detected in blood for 6 months after treatment) to drug therapy. Since the liver has incredible regenerative ability, achieving SVR as quickly as possible is important because some liver damage can be reversed if the cause of the damage is removed.
Staying Healthy with Hepatitis
Not everyone needs treatment right away, but it’s important to be monitored regularly by an experienced doctor and discuss treatment options of the best way to keep you healthy.
- Get vaccinated against Hepatitis A and Hepatitis B
- Avoid alcohol and drugs
- Eat a healthy & balanced diet. Include a lot of vegetables and fruits; try to stay away from too much salt, sugar and fat.
- Exercise regularly. Walking is one of the best exercises, and it helps to make you feel less tired.
- Check with a health professional before taking any prescription pills, supplements, or over-the-counter medications.
- Do not share razors, nail clippers, needles or other items that come in contact with blood with other people.